
Medical Malpractice: Misdiagnosis versus Delayed Diagnosis
Misdiagnosis and delayed diagnosis are two of the most common (and damaging) forms of medical malpractice. Some reports suggest that as many as 40% of medical
Home » Patient Safety Blog » Informed Consent: It Might Not Mean What You Think
As a New York Medical Malpractice Attorney, I deal with people all the time who have terrible, often life altering, injuries from medical errors.
Occasionally, I have heard from clients that they do not even know what went wrong.

While medical issues can sometimes be complex, it is the doctor’s job to explain things in a way that patients understand.
Therefore, the requirement of being able to dispel a patient’s confusion is at the heart of informed consent laws.
In order to meet the requirements of the law, informed consent mandates that patients understand the kind of treatment they are agreeing to.
Simply put, this means a patient must understand the risks, benefits, and alternatives of the treatment being contemplated.
The overarching consideration is that it is the patient’s right to direct the course of treatment he or she is to undergo.
The legal requirement for obtaining informed consent rests with the treating physician.
A physician may delegate that duty to another health professional.
However, if something goes wrong and the delegated person fails to sufficiently inform the patient of the risks, benefits and alternatives to the treatment contemplated, then the physician is still responsible.
To obtain a valid informed consent, your doctor must explain each of these items to you.
Of course, there are exceptions in emergency situations.
If immediate treatment is necessary to prevent death or serious harm, then a doctor can act in his or her own best judgment if delaying treatment to obtain consent might cause an additional injury.
Also, if the patient is a minor and a family member cannot be contacted in a timely manner, this is an exception as well.
We all rely on our doctors to give us the best treatment when we are sick.
But that does not mean doctors can automatically decide what is best for us without discussing the options.
After all, it is the patient’s own health, or even life, that is at stake.
It is clearly both a legal and ethical requirement to get a patient’s informed consent to medical treatment.
However, recent studies have shown that this is not always done.
For example, a study by the Journal of General Internal Medicine found that with coronary artery stents used with certain types of heart disease, only 10% of patients were offered alternative options by their doctors.
Of these patients, 77% reported that their doctor explained the reasons for having a stent, but only 19% said the downsides of the procedure were discussed.
In the end, only 16% of these heart patients were asked what their treatment preferences were.
Unfortunately, the heart stent issues are not isolated.
Many patients with various medical issues are not getting all of the information they need.
Did you know that in New York, the rules about obtaining informed consent only apply to “invasive procedures”?
This news comes as a big surprise to many people, particularly in the context of breast cancer.
The Informed Consent provisions that are codified in Public Health Law § 2805-d specifically state:
Ҥ 2805-d. Limitation of medical, dental or podiatric malpractice action based on lack of informed consent.
1. Lack of informed consent means the failure of the person providing the professional treatment or diagnosis to disclose to the patient such alternatives thereto and the reasonably foreseeable risks and benefits involved as a reasonable medical, dental or podiatric practitioner under similar circumstances would have disclosed, in a manner permitting the patient to make a knowledgeable evaluation.
2. The right of action to recover for medical, dental or podiatric malpractice based on a lack of informed consent is limited to those cases involving either
(a) non-emergency treatment, procedure or surgery, or
(b) a diagnostic procedure which involved invasion or disruption of the integrity of the body.”
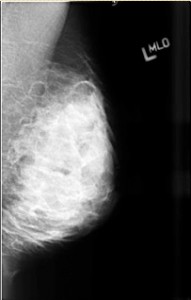
So for example, mammography has been shown to miss 52% of cancer in women with dense breasts.
This is a horribly substandard detection rate.
And it seems that everyone (except the American College of Radiology) finds this unacceptable.
In fact, it is worse odds than a pure coin toss.
So imagine the shock that so many women – who aren’t diagnosed with breast cancer until it’s at an advanced stage – feel when they learn of this information for the first time.
Many of these women feel they weren’t properly “informed”, and I believe they are 100% correct.
Consider also that when mammography is used in conjunction with breast ultrasonography, the breast cancer detection rate increases to 97%.
That of course is a much more acceptable rate of detection and one that everyone would prefer.
However, there is no violation of the informed consent requirements for these women who aren’t told of this risk (that mammos will miss 52% of cancers), or the alternatives (doing a non-invasive breast ultrasound or MRI will increase the detection rate to 97%).
Again, informed consent in New York only applies to invasive procedures.
Since a mammography is not a diagnostic test that involves the “invasion or disruption of the integrity of the body”, medical malpractice defense lawyers argue that women are not required to be told of the alternatives to mammograms such as breast ultrasonography or breast MRIs under the law of informed consent here in New York.
Shouldn’t doctors be required by law to explain all the risks, benefits, and alternatives to all medical treatment in a way that each patient understands?
Here, at The DiPietro Law Firm, we’re committed to helping victims of sexual abuse and assault find the justice they deserve.
All information discussed during our consultations always remains completely 100% confidential.
Would you like our help?
Founder Anthony T. DiPietro, Esq. is a compassionate and skilled trial attorney who has completely dedicated the past 23 years of his career to litigating medical malpractice and sexual abuse cases against major corporate institutions including hospitals, medical clinics, schools, and other wrongdoers.
Mr. DiPietro has also obtained some of New York State’s highest verdicts and settlements, and has been selected to New York State Super Lawyers® each year, for the past 10 years in a row.
In 2022, Mr. DiPietro was selected as one of America’s Top 100 High-Stakes Litigators for the landmark cases he’s won on behalf of survivors of sexual exploitation and abuse.
Here, at The DiPietro Law Firm, we’re committed to helping victims of sexual abuse and assault find the justice they deserve.
All information discussed during our consultations always remains completely 100% confidential.
Would you like our help?

Misdiagnosis and delayed diagnosis are two of the most common (and damaging) forms of medical malpractice. Some reports suggest that as many as 40% of medical

A column caught my eye earlier this month which discusses in detail the problems patients are having obtaining adequate information about their own care. In
Years of Abuse: 1987 – 2016
Brief:
Robert Hadden, a disgraced Obstetrician-Gynecologist (OB/GYN) who worked for Columbia University and NewYork-Presbyterian Hospital, was criminally convicted in 2016 of sexually exploiting and abusing patients under the guise of medical care.
Hadden used his position of authority and trust to sexually exploit women and girls for nearly three decades as a Columbia University physician.
All the while, Columbia University and New York-Presbyterian Hospital administrators turned their backs and ignored reports of Hadden’s abuse, gaslighting patients and the public.
Read More:
Years of Abuse: 1979 – 2022
Brief:
David H. Broadbent is a former OB/GYN under criminal investigation and facing civil lawsuits for sexual abuse of patients.
Broadent worked at multiple medical facilities in the Provo, Orem and Salt Lake City, UT areas.
These facilities included Intermountain Healthcare’s Utah Valley Hospital, MountainStar Healthcare’s Timpanogos Hospital, other Utah health care providers, and he also had adverse action taken against his medical license back in 1990.
Read More:
Years of Abuse: 1990 – 2016
Read More: University of Southern California & Predator George Tyndall
Years of Abuse: 1961 – 1996
Brief:
22 predator teachers and administrators, over the course of 35 years.
Years of Abuse: 1960 – 1982
If you have any questions about whether or not you have a case, or just want to obtain more information about what you’ve experienced – feel free to contact us through our secure website chat.
You can also contact us by calling us at (212) 233-3600 or toll free at (800) 215-1003.
All of our consultations are free and 100% confidential. Thank you.
All Rights Reserved ©2023 by The DiPietro Law Firm